Her relapse into melancholy felt like defeat—nevertheless it provided very important clues to reaching lasting psychiatric reduction.
The 67-year-old girl from Alabama had already endured 4 main depressive episodes in her decades-long battle with psychological sickness. After exhausting quite a few medications and different therapies, in 2015 she turned to an experimental final resort: deep brain stimulation, or DBS.
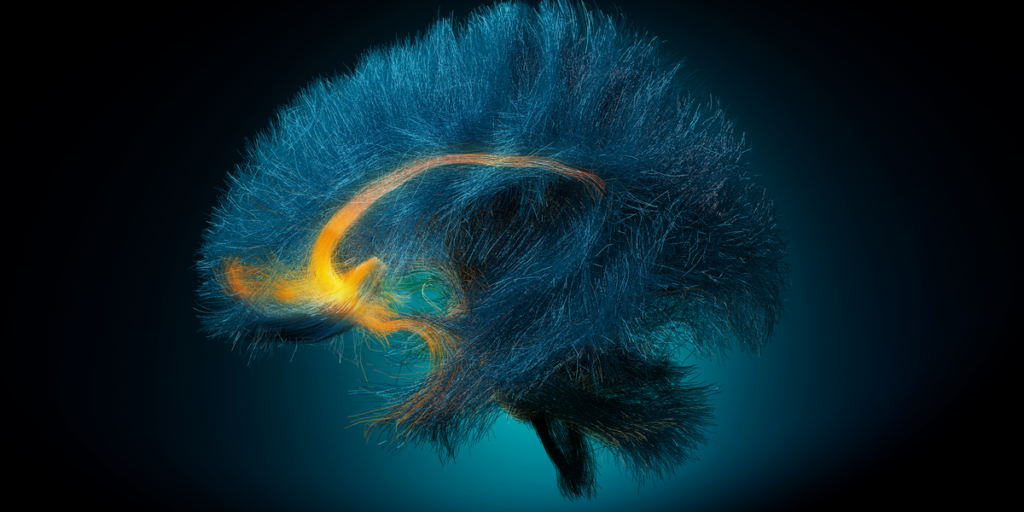
Neurosurgeons implanted electrodes a number of inches under her cranium, focusing on a small bundle of neural fibers in a mind area behind the brow that acts as an important hub for temper regulation. Skinny wires linked the electrodes to a pulse generator discreetly inserted in her higher chest. As soon as activated, the gadget delivered a gentle stream of high-frequency electrical energy, gently buzzing the focused circuits to disrupt maladaptive patterns and, like a pacemaker for the mind, restore a more healthy steadiness of neural exercise.
At first, the remedy gave the impression to be working. The lady’s despair lifted, and he or she edged nearer to remission. Watching football for hours along with her husband on Sundays began to really feel tedious—in a great way. Her want to get off the sofa and pursue different actions had returned.
An X-ray picture reveals two pairs of DBS electrodes implanted for melancholy remedy. Division of Neurosurgery, Baylor Faculty of Medication
However 4 months on, the darkness crept again in. The lady’s sudden downturn blindsided the medical workforce that had been carefully monitoring her restoration. The medical doctors needed to make three changes to the implant’s stimulation parameters, slowly growing the voltage, earlier than her situation lastly stabilized—an agonizing couple of months.
When the clinicians reviewed the information later, they realized that the electrodes embedded within the girl’s mind had detected bother brewing earlier than she did. Refined shifts within the electrical patterns coursing by means of her neural fibers had flagged the approaching relapse weeks earlier than her outward signs reappeared. If clinicians had acted on these alerts, they could have adjusted the stimulation settings in time to forestall her relapse.
It’s a thought that weighs on Patricio Riva Posse, the psychiatrist at Emory College Faculty of Medication, in Atlanta, who handled the girl. Trying again now, he says, had he identified that the mind’s circuits had been off-kilter, “I might have taken motion earlier.”
Happily, Riva Posse not has to dwell on what might have been. Along with colleagues on the Icahn Faculty of Medication at Mount Sinai, in New York City, and Georgia Tech, in Atlanta, he’s now leveraging advances in DBS {hardware} and artificial intelligence (AI) to design extra exact remedies for melancholy. The workforce’s purpose is to base remedy on goal neural knowledge fairly than the subjective measures—affected person accounts, scientific hunches, questionnaires, temper scales—that dominate psychiatry immediately.
The pioneering neurologist Helen S. Mayberg co-led the workforce with Riva Posse and Christopher Rozell of Georgia Tech. In the end, they hope to allow preemptive interventions fairly than regretful, after-the-fact changes.
It’s a brand new frontier for psychiatry. The sector has lengthy been one of many few medical disciplines with out goal measures to information remedy selections. However with the appearance of real-time mind monitoring with AI-driven analytics, that would lastly change. “It’s a complete totally different mindset now,” says Martijn Figee, a Mount Sinai psychiatrist concerned within the analysis. “My instinct, sadly, just isn’t one hundred pc [accurate],” he acknowledges. “So finally, I might at all times belief the mind extra.”
Researchers are growing “an automated alarm system”—an AI-driven device designed to repeatedly monitor gadget output and flag warning indicators of relapse.
Different analysis teams are pursuing comparable targets, aiming to maneuver past the one-size-fits-all strategy that has lengthy outlined DBS remedy for mental health and exchange it with exact stimulation tailor-made to particular person wants. Whereas standardized protocols profit around 60 percent of individuals with treatment-resistant melancholy, they nonetheless depart a considerable minority with out significant reduction.
No DBS platform is but accredited for treating melancholy, though some first-generation gadgets are getting shut. These are rooted in decades-old know-how, nonetheless, whereas the Mount Sinai workforce and others are breaking new floor. They’re investigating analytical frameworks that harness mind knowledge to foretell relapses, optimize stimulation parameters, or dynamically modify gadget output in a responsive, closed-loop method.
“The sector is simply at a brilliant thrilling place,” says Benjamin Davidson, a neurosurgeon on the Sunnybrook Well being Sciences Centre, in Toronto. “Issues are beginning to transfer at a form of dizzying tempo.”
The Origins of DBS for Melancholy
That momentum is a comparatively current phenomenon in a area that, for the previous twenty years, has progressed by means of child steps. Beset by industrial and scientific setbacks, little has modified over time other than the adoption of newer surgical strategies. The most important advance was an imaging-guided surgical strategy known as tractography that enables for greater precision in electrode placement, knowledgeable by connectivity patterns between bundles of mind fibers fairly than anatomical landmarks alone.
“The story is one among iteration to optimize and refine the focusing on utilizing new neuroscience instruments,” says Mayberg, who launched the world’s first DBS trial for treatment-resistant depression within the early 2000s on the College of Toronto. “The process, as envisioned and revealed in 2005, is, in essence, what we proceed to do immediately,” she says.
DBS is primarily used to handle motion problems corresponding to important tremor and Parkinson’s disease. For these illnesses, it’s a longtime and accredited therapy that may drastically cut back signs corresponding to shaking and muscle rigidity.
However Mayberg was impressed by the invention of a mind area known as the subgenual cingulate (SGC), which performs a key role in acute sadness and the effects of antidepressant treatments. She theorized that stimulating this space would possibly alleviate extreme, treatment-resistant melancholy. Her sufferers had been individuals who had sometimes tried a number of sorts of antidepressant drugs and extra drastic measures, like electroconvulsive remedy, with out discovering any reduction.
Whereas the remedy didn’t work for everybody, many did really feel higher. Six months after surgery, 12 of the 20-person cohort skilled a profound lifting of their depressive signs, with 7 going into full remission. The impact was lasting, with a lot of these people persevering with to report advantages to today, based on Andres Lozano, the College of Toronto neurosurgeon who carried out the operations.
Mayberg’s speculation, it will appear, had proved appropriate.
Studying from DBS Failures
But, for all its early potential, DBS by no means gained traction as a mainstream psychiatric remedy. It’s often used immediately for folks with debilitating obsessive-compulsive dysfunction, however the approach stays unapproved for melancholy and is basically confined to analysis trials—a few of which have led to dispiriting, high-profile failure.
One of the notable setbacks occurred in 2013. The gadget firm St. Jude Medical got down to replicate the findings of Mayberg’s examine in a randomized trial, with plans to enlist 200 contributors. However the study was halted prematurely after solely 90 sufferers had been enrolled. An interim evaluation had discovered the remedy was no simpler than sham stimulation.
It was a crushing blow to the sector. Mayberg and others struggled to proceed their analysis, as funding companies and the scientific group at giant grew more and more skeptical in regards to the viability of DBS for melancholy.
With the good thing about hindsight, nonetheless, many researchers now consider that the St. Jude failure owed extra to the examine’s design flaws than to any inherent shortcomings of DBS itself. An extended-term follow-up of contributors indicated that the remedy’s antidepressant impact steadily strengthened. The trial might merely have measured responses on the unsuitable timeline. Plus, the neurosurgical placement of the DBS electrodes relied on an outdated understanding of mind connectivity, resulting in suboptimal positioning. This may occasionally have delayed the therapeutic response previous the preliminary 6- to 12-month evaluation window.
These missteps seemingly undermined the examine’s outcomes, the trial investigators later concluded. However with the suitable trial design, most consultants anticipate that future research will succeed. “That might make an enormous distinction,” says Darin Dougherty, a psychiatrist at Massachusetts Normal Hospital, in Boston. “Hopefully these classes discovered can be sufficient to get it excessive.”
 A affected person recognized as Sarah participates in a trial at UC San Francisco of the primary absolutely closed-loop DBS system for melancholy. Maurice Ramirez
A affected person recognized as Sarah participates in a trial at UC San Francisco of the primary absolutely closed-loop DBS system for melancholy. Maurice Ramirez
The biomedical firm Abbott (which acquired St. Jude in 2017) is now conducting a do-over examine at 22 websites throughout the United States; Dougherty, Figee, Riva Posse, and different leaders within the area are concerned within the effort. The 100-person trial, launched in September 2024, might lastly result in regulatory approval and wider-scale adoption of DBS as a remedy technique for melancholy.
However Abbott’s examine takes a “set-it-and-forget-it” strategy, wherein stimulation parameters are programmed throughout preliminary visits and stay largely unchanged over time. The settings are usually standardized throughout sufferers, with a typical pulse width and frequency mounted at round 90 microseconds and 130 hertz, respectively. Solely the amplitude of stimulation, measured in volts, is often adjusted to accommodate particular person tolerances or symptom severity.
Whereas this remedy strategy is straightforward and scalable, it lacks the adaptability to answer the dynamic nature of melancholy and its various signs from one particular person to the subsequent. This limitation stems partially from a technological shortcoming of the Abbott platform: It might probably ship exactly tuned electrical energy, nevertheless it lacks the power to sense and file neural exercise. With out this suggestions mechanism, the gadget can’t detect shifts in mind states that may sign a relapse or a necessity for parameter changes, leaving clinicians reliant on sufferers’ reviews.
In distinction, newer DBS gadgets for epilepsy and motion problems can each stimulate and file alerts. Medtronic’s Percept system and NeuroPace’s Responsive Neurostimulator, for instance, provide real-time suggestions capabilities, which might permit for extra adaptive therapies. Researchers wish to convey that flexibility to DBS for melancholy.
How Responsive DBS for Melancholy Works
Contemplate once more the instance of Riva Posse’s 67-year-old affected person. As described in Nature two years ago, this girl acquired a research-grade model of the Percept platform that detected indicators of neural instability 5 weeks earlier than her scientific signs reappeared.
“Earlier than the affected person knew something was unsuitable—earlier than there was even a touch of habits that would appear symptomatic of a relapse—the mind sign was headed within the unsuitable route,” says Rozell, the neuroengineer at Georgia Tech who developed the AI mannequin used to interpret the girl’s mind exercise patterns.
Rozell’s mannequin mixed a neural community classification scheme (for analyzing mind alerts) with a generative causal explainer (for figuring out key exercise patterns). His work uncovered a definite biomarker that reliably differentiated between states of melancholy relapse and restoration. Intriguingly, the biomarker also reflected changes in sleep quality, a telling early indicator since poor sleep patterns typically precede the return of melancholy signs.
Melancholy can take many varieties: Some folks expertise it as emotional despondency, whereas others battle with obsessive ideas or a lack of pleasure.
However the insights offered by Rozell’s mannequin got here too late to assist the affected person within the second—they had been validated solely after her relapse had occurred. To deal with this limitation, the researchers are actually refining the strategy for real-time use, aiming to develop what Mayberg calls “an automated alarm system”—an AI-driven device designed to repeatedly monitor gadget output and flag warning indicators of relapse.
Such a system might immediate clinicians to intervene earlier than these mind alerts escalate right into a full-blown depressive episode. Concurrently, it might filter out false alerts from sufferers, offering reassurance to customers who would possibly in any other case interpret regular stress or nervousness as indicators of an impending relapse. Knowledgeable by this neurofeedback, psychiatrists would possibly then select to fine-tune stimulation settings. Or they could proactively advocate extra assist, corresponding to psychotherapy or treatment changes.
Closing the Loop for DBS
Going one step additional, researchers from the College of California, San Francisco, are exploring a totally closed-loop DBS system for melancholy that removes among the want for human decision-making. Their strategy empowers the gadget itself to robotically modify stimulation parameters in actual time primarily based on mind exercise.
Reporting on their first affected person—a lady in her 30s named Sarah, who withheld her final title for privateness—the UC San Francisco workforce documented transformative improvements in her temper, emotional steadiness, on a regular basis functioning, and general outlook on life, all within the first week after the implant was switched on.
 Sarah reviews that the closed-loop DBS system restored pleasure and function to her life. John Lok
Sarah reviews that the closed-loop DBS system restored pleasure and function to her life. John Lok
“My life took an instantaneous upward flip,” Sarah stated at a 2021 press convention saying the examine’s early findings. “Hobbies I used to distract myself from suicidal ideas instantly turned pleasurable once more. I used to be in a position to make small selections about what to eat with out turning into caught in a morass of indecision for hours,” she stated, including, “the gadget has stored my melancholy at bay, permitting me to return to my greatest self and rebuild a life value dwelling.”
In accordance with Andrew Krystal, the UC San Francisco psychiatrist main the trouble, comparable advantages have since been seen in at the very least two different recipients of the closed-loop DBS gadget.
In every case, sufferers first bear an intensive 10-day exploration of their typical neural exercise, with 10 electrodes—focusing on 5 places on all sides of the mind—quickly implanted. Throughout this era, researchers administer a battery of checks to establish the best websites for each stimulation and sensing. As soon as the optimum places are decided, a second surgical procedure is carried out to implant the everlasting DBS system, now simplified to only two electrodes: one devoted to delivering stimulation and the opposite to recording neural exercise.
When the recording electrode detects mind exercise related to melancholy—an occasion that may occur a whole lot of occasions per day—it prompts the opposite electrode to ship a short burst of electrical energy lasting a number of seconds. This strategy stands out not solely as a result of it operates robotically in response to real-time mind exercise, but in addition as a result of it employs intermittent, on-demand stimulation fairly than the continual stimulation extra generally employed in DBS for psychiatric situations.
This adaptive and dynamic suggestions technique could also be particularly effectively suited to addressing the day-to-day fluctuations in temper and emotional pressure that may make melancholy so arduous to stay with, notes Katherine Scangos, a psychiatrist who participated within the examine. Sufferers have advised her that receiving stimulation at key moments—like throughout a nerve-racking interplay on the checkout line of a grocery retailer—helped forestall them from spiraling into misery. “They may actually inform that they had been getting the stimulation once they wanted it most,” says Scangos, who joined the workers of the College of Pennsylvania final 12 months.
Figuring out the suitable websites and parameters is an intricate and labor-intensive course of, and it’s not at all times instantly clear which settings will work greatest, based on UC San Francisco neurosurgeon Kristin Sellers. All the information they accumulate creates a “curse of bounty,” she says. But, in her view, the outcomes reveal the effectiveness of taking this customized strategy. “Nobody has an similar implant,” she says.
New Concepts on DBS for Melancholy
In the meantime, a workforce at Baylor Faculty of Medication, in Houston, is pursuing a unique strategy to personalised DBS for melancholy. The workforce’s standardized implant consists of two coordinated units of electrodes: One targets the SGC mind area concerned in profound disappointment, whereas the opposite stimulates a reward-and-motivation hub deep within the mind’s basal ganglia.
The customization occurs on the entrance finish throughout the preliminary surgical process, when clinicians quickly place one other 10 electrodes into the mind that take recordings by way of electroencephalography (EEG). This methodology tracks mind waves and, as sufferers bear numerous checks and actions, permits the Baylor workforce to map related neural networks and connections. On the identical time, the medical doctors can fiddle with the amplitude, pulse width, frequency, and form of the stimulation area.
“Then we will principally design bespoke stimulation parameters for that particular person which are going to maneuver that particular person’s community in the suitable route,” explains Sameer Sheth, the neurosurgeon main the mission. Sheth and his colleagues have handled seven folks, with promising initial results.
Any of those extremely individualized approaches will contain extra surgical procedures and prolonged stays within the hospital. However as Dougherty of Massachusetts Normal Hospital factors out, “We have to do that invasive analysis first in order that we’d be capable to use noninvasive approaches later.”
He imagines a future wherein electrodes on the scalp or superior imaging strategies might establish optimum targets and information remedy changes. Even then, nonetheless, if DBS requires extremely customized programming, it will likely be difficult to make it accessible to the tens of millions of individuals worldwide within the throes of melancholy.
“The query will at all times be in regards to the scalability of issues,” says Volker A. Coenen, a neurosurgeon on the College of Freiburg Medical Heart, in Germany. Coenen is subsequently focusing his power on testing a standardized DBS protocol, one which entails implanting the Vercise Gevia system from Boston Scientific into an space of the mind generally known as the medial forebrain bundle.
In his view, this mind area provides a extra direct and environment friendly pathway to reward programs and emotional-regulation networks. Nonetheless, the varied mind areas into consideration are all interconnected, which explains why all of them appear to supply some extent of therapeutic profit. “You may perturb the community from totally different angles,” Coenen says.
The Street Forward for DBS
So, which web site is greatest? The reply seemingly will depend on the particular signs and underlying mind circuits distinctive to every particular person, says Alik Widge, a psychiatrist and biomedical engineer on the College of Minnesota, in Minneapolis.
“There’s no such factor as DBS for melancholy. There’s DBS for treating particular cognitive-emotional syndromes,” he argues—and totally different targets can be suited to accessing totally different features of the dysfunction. Melancholy can take many varieties: Some folks expertise it as emotional despondency, whereas others battle with obsessive ideas or a lack of pleasure.
The optimum stimulation methodology might also differ. Steady stimulation may match greatest for folks whose melancholy follows a gentle, persistent course, whereas intermittent or responsive stimulation could also be extra applicable for these whose signs fluctuate with each day ups and downs. “It’s just like the distinction between climate and local weather,” says Riva Posse—some folks may have an umbrella for passing showers, whereas others want to bolster their houses in opposition to rising tides.
In the end, whether or not they’re tweaking stimulation parameters, discovering one of the best mind targets, or making stimulation reply to real-time mind alerts, the purpose for researchers within the area stays the identical: to create a neurologically exact strategy to treating melancholy in individuals who have discovered no reduction. “There are such a lot of levers we will press right here,” says Nir Lipsman, who directs the Harquail Centre for Neuromodulation at Sunnybrook, in Toronto. He’s assured that at the very least a few of these efforts will unlock new therapeutic prospects.
“The sector is experiencing a form of reset,” Lipsman provides. Now, with neural exercise as a information, the brains of individuals present process DBS ought to likewise expertise a form of reset as effectively.
From Your Website Articles
Associated Articles Across the Internet